Introduction
A stroke occurs when a part of the blood supply to the brain is cut off and brain cells cannot receive oxygen. Eventually, brain cell death occurs. Every year about 550,000 people in the United States suffer from a stroke. About 150,000 people die annually from strokes, making it the third leading cause of death in the U.S. after heart disease and cancer.
There are two main types of stroke: ischemic stroke and hemorrhagic stroke. Ischemic stroke occurs when blood clots or cholesterol deposits occlude vessels that supply blood to the brain. Occlusions may form within the vessels in the brain, or the clots can form outside of the brain, most of the heart, and then travel to the brain (embolization). Hemorrhagic stroke results from ruptured blood vessels inside the brain or on the brain's surface.
Risk Factors
There are many risk factors which may contribute to stroke including high blood pressure, diabetes, heart disease, high cholesterol, smoking, obesity, sleep apnea, and illicit drug use. The presence of narrowing, due to atherosclerotic disease, in the carotid arteries (carotid stenosis) and the arteries within the brain (intracranial atherosclerosis) can also increase the risk of having a stroke. The incidence of stroke rises with age, particularly over the age of 60. A previous stroke warning or transient ischemic attack (TIA) representing a temporary decrease in blood flow to an area of the brain, and a family history of stroke, are also risk factors. In patients under the age of 50, the causes of stroke differ from those in older individuals and may include heart disease including infections (endocarditis), congenital or acquired aortic or mitral valvular abnormalities, arrhythmias (especially atrial fibrillation that may be intermittent), and heart muscle pathology (cardiomyopathy) with congestive heart failure. Inflammatory disease of blood vessels, hematologic abnormalities and hypercoagulability and traumatic injuries to blood vessels causing dissection are others to consider. There are many factors underlying hemorrhagic strokes but they may occur with rupture of an aneurysm, an arteriovenous malformation (AVM) which is an abnormal tangle of blood vessels in the brain, head injury, hypertensive small blood vessel disease, or rare disorders of small blood vessels like amyloidosis.
Symptoms
The symptoms of a stroke can vary widely depending on the part of the brain affected but they are usually abrupt in onset. Some patients experience a tingling or weakness in the arms or legs, usually on one side of the body. Strokes can also cause sudden changes in vision such as loss of vision in one eye, loss of ability to see to one side, or double vision. Some individuals suddenly lose their ability to speak clearly or coherently or they may have difficulty understanding spoken or written language. A person with a stroke may experience a loss of balance, loss of consciousness, dizziness or a severe headache.
Diagnosis
Evaluation for a possible stroke is done urgently in the hospital by physical and neurological examination, computed tomography (CT) scans of the brain or magnetic resonance imaging (MRI). Another important tool for assessing patients with a recent stroke is ultrasound testing of the blood flow to the brain and within the brain. This can be done non-invasively with a Transcranial Doppler (TCD) and Carotid Duplex ultrasound. These ultrasound tests are also helpful in evaluating patients who have had symptoms of transient ischemic attacks indicating reversible poor circulation to the brain (carotid stenosis) and in following patients who have been found to have blockages in their arteries supplying the brain (intracranial atherosclerosis).
Treatment
Treatment of a stroke is an emergency and should be administered as soon as possible after the onset of symptoms to optimize the efficacy. The most common treatment for stroke is antiplatelet therapy (aspirin, clopidogrel) that "thin" the blood. These are often used to prevent a further stroke event. Thrombolytic agents such as TPA (tissue plasminogen activator), administered in the emergency room, are used within the first 3-6 hours of a new stroke and can aid in dissolving the clot causing the stroke to improve the chances of recovery. Newer techniques to extract clots from occluded blood vessels in the brain are also available at certain stroke centers. It is therefore critical to get to the emergency room as quickly as possible if one suspects they or someone they know is having a stroke so that these treatments can be considered. Aneurysms and AVMS’s can be treated surgically or with less invasive interventional neuroradiological procedures to lower risk of new or recurrent bleeding.
Summary
Stroke is an emergency. It is often said where stroke treatment is concerned “Time is Brain.” The term “brain attack” as an analogy to “heart attack” has been popularized to emphasize the critical time sensitivity of implementing effective treatment. There are many treatments available but if you suspect that you may be having a stroke, it is vital to call 911 and get to the nearest hospital. Our neurologists are experienced in helping you to prevent stroke and to recover afterwards.
One mnemonic for self-assessment for a possible stroke is:
B.E. F.A.S.T.—the Balance, Eyes, Face, Arm and Speech Test
Remembering B.E. F.A.S.T. is an easy way to quickly identify the early warning signs of a stroke.
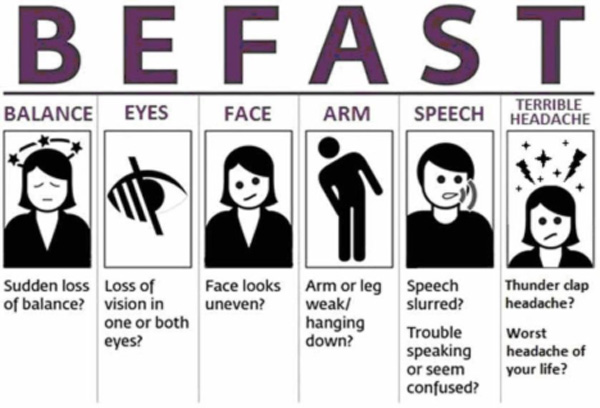
Know the signs, and B.E. F.A.S.T. if you suspect stroke!
The final “T” in BE FAST should also stand for TIME!!!!
Remember, every minute counts. Do not wait. Call 911.